What is Mycoplasma Testing ?
Mycoplasma Testing is used to detect the presence of mycoplasma contamination in cell cultures, biological products, and manufacturing processes involving living cells. Mycoplasmas are a unique group of bacteria lacking a cell wall, which allows them to evade standard filtration and remain undetected by conventional sterility tests. Their presence can alter cellular metabolism, compromise experimental results, and pose significant risks to the safety and efficacy of biopharmaceutical products.
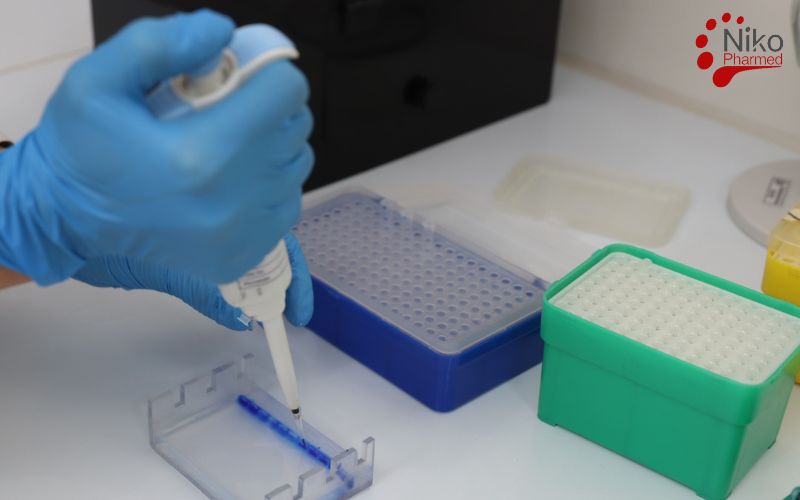
The Mycoplasma Testing process typically involves culturing samples in specialized media that support the growth of mycoplasmas, followed by microscopic examination and extended incubation under controlled conditions to ensure accurate detection. This method ensures that biological materials meet stringent safety standards before being released for clinical or commercial use. In routine microbiological quality control, mycoplasma-specific assays are often performed alongside bioburden testing to monitor both total viable microbial load and hard-to-detect wall-less organisms in cell cultures and biopharmaceutical manufacturing.
International Standard of Mycoplasma Testing
The standard method for detecting mycoplasma contamination in biological products and cell cultures is established under USP <63>. This compendial chapter outlines validated procedures for the cultivation, detection, and identification of mycoplasmas using both liquid and solid media, microscopic examination, and specified incubation conditions.
Compliance with USP <63> ensures that products meet regulatory requirements for microbiological safety and are free from mycoplasma contamination that could compromise product integrity or patient safety. For parenteral biologics and cell-based therapies, mycoplasma control is commonly complemented by Bacterial Endotoxin Testing (BET) to address both microbial contamination and pyrogenic endotoxin risk in accordance with pharmacopeial requirements.
Mycoplasma Testing Procedure
Mycoplasma testing, as described by pharmacopeial standards, employs two primary methodologies—traditional culture-based techniques and nucleic acid amplification via polymerase chain reaction (PCR)—to ensure sensitive and specific detection of mycoplasma contamination in cell substrates and biological products.
These methods target the unique biological and physiological characteristics of mycoplasmas, a group of pleomorphic, wall-less prokaryotes from the class Mollicutes, which includes over 200 species, with Mycoplasma orale, M. arginini, and Acholeplasma laidlawii being the most commonly encountered contaminants in biomanufacturing.
Traditional Cultivation Method
The culture-based method, considered the gold standard for viability detection, involves the use of both liquid (broth) and solid (agar) mycoplasma-specific media. The media are typically rich in nutrients such as peptones, yeast extract, serum (e.g., horse or bovine serum), and DNA precursors, and are buffered to maintain a pH of approximately 7.8. The addition of antibiotics (e.g., penicillin or thallium acetate) helps suppress the growth of competing bacteria while allowing mycoplasma proliferation.
Procedure
A test sample (minimum 1 mL, ideally 10 mL) is inoculated into mycoplasma broth and incubated at 35–37°C in a 5–10% CO₂ humidified atmosphere for up to 14–28 days.
Subcultures are taken from the broth at regular intervals (typically every 3–7 days) and plated onto solid agar.
Agar plates are incubated under the same conditions and examined microscopically at multiple time points (e.g., days 7, 14, 21, and 28).
Microscopic Examination:
Using phase-contrast microscopy (typically 200–400× magnification), colonies are identified by their distinct “fried-egg” morphology—comprising a dense central core and a lighter periphery due to subsurface growth into the agar.
Sensitivity and Detection Limit
The culture method is capable of detecting as few as 10 colony-forming units (CFU) per mL.
Detection depends on the growth characteristics of different species, with fast-growing species such as M. arginini detectable within 3–7 days, while slower-growing species like M. hyorhinis may require the full 28-day incubation.
The method detects only viable organisms, which is critical for assessing the actual risk of contamination.
Polymerase Chain Reaction (PCR) Method
The PCR method is based on the amplification of conserved regions within the mycoplasma genome, typically the 16S ribosomal RNA (rRNA) gene or the 23S rRNA gene. These genes are highly conserved among mycoplasma species but sufficiently divergent from those of other bacteria to allow specific detection.
Procedure
DNA is extracted from the test sample using silica column- or magnetic bead-based purification to remove PCR inhibitors.
Specific primers targeting conserved sequences (e.g., 16S rDNA region between bases 340–450) are used in a standard or real-time PCR assay.
Amplification involves 30–40 cycles of denaturation (~95°C), annealing (~55–60°C), and extension (~72°C).
Amplicons (typically 200–500 base pairs) are analyzed by gel electrophoresis or quantitative fluorescence in real-time PCR.
Controls and Validation
Positive controls consist of synthetic DNA or heat-inactivated known mycoplasma strains to confirm amplification efficiency.
Negative (no-template) controls are included in every run to check for contamination.
The assay must be validated for:
- Sensitivity: Typically down to 10 genome copies per reaction (approx. 10²–10³ CFU/mL equivalency).
- Specificity: Cross-reactivity must be ruled out using BLAST analysis and testing against non-mycoplasma DNA.
- Robustness: The method must resist inhibition by components such as serum, antibiotics, and preservatives.
Advantages and Limitations
PCR provides rapid results (within 1–2 days) and detects both viable and non-viable organisms.
It may fail to detect highly divergent or rare mycoplasma species if primers are not sufficiently broad-spectrum.
False positives can result from carryover contamination; hence, strict contamination controls (e.g., uracil-DNA glycosylase systems) are often employed.
| Parameter | Cultivation Method (Traditional) | PCR Method (Molecular) |
|---|---|---|
| Principle | Detection of viable mycoplasma through growth on selective media | Detection of mycoplasma DNA through amplification of genetic material |
| Detection Target | Viable mycoplasma organisms | DNA from viable and non-viable mycoplasmas |
| Media Used | Broth (e.g., SP4, Frey’s) and solid agar media | None (requires nucleic acid extraction buffers) |
| Incubation Conditions | 35–37°C, 5–10% CO₂, up to 28 days | Thermal cycling (PCR machine), 1–2 hours per run |
| Time to Results | 23–28 days | 8–10 days |
| Sensitivity | ~10 CFU/mL | ~10–100 genome copies per reaction |
| Specificity | High (for viable strains that grow in vitro) | Very high (depends on primer design; may miss unknown species) |
| Species Detected | Common viable species (e.g., M. orale, M. arginini, A. laidlawii) | Broad range, including non-cultivable and fastidious species |
| Controls Required | Positive control strain, negative control media | Positive DNA control, negative (no-template) control, inhibition control |
| Detection Method | Visual/microscopic observation of colonies | Gel electrophoresis or real-time fluorescence detection |
| False Negatives Risk | High if slow-growing or non-viable mycoplasmas are present | Possible if PCR inhibitors or poor DNA extraction |
| False Positives Risk | Low (rare contamination in media) | Higher (DNA contamination risk in lab environment) |
| Validation Requirements | Growth promotion, sensitivity testing | Limit of detection, specificity, robustness, inhibition control |
| Regulatory Acceptance | Widely accepted, compendial method | Accepted with proper validation and as a rapid alternative |
| Cost and Resources | Lower equipment cost, higher labor and time | Higher equipment cost, rapid turnaround |
| Use Case | Confirmatory testing for viable contaminants | Rapid screening, especially in time-sensitive workflows |
Why Choose Nikopharmad for Your Mycoplasma Testing Needs?
ILAC Accreditation & ISO 17025 Certification
Nikopharmad Laboratory is accredited under the ILAC mutual recognition arrangement and fully compliant with ISO/IEC 17025 standards. This certifies both our technical proficiency and quality assurance systems, ensuring that your mycoplasma test data is recognized by regulatory authorities including the FDA, EMA, PMDA, and TÜV—facilitating seamless global submissions and product approvals.
Comprehensive Mycoplasma Detection Methods
We offer validated mycoplasma testing using both compendial culture-based methods and rapid molecular techniques (PCR), fully aligned with USP <63>, EP 2.6.7, and JP guidelines. Our testing platform includes dual-method detection to identify a wide spectrum of Mycoplasma and Acholeplasma species, covering viable, non-viable, and fastidious organisms with or without pre-enrichment.
Expert Scientific Team & Advanced Laboratory Infrastructure
Our team of microbiologists, molecular biologists, and quality experts brings decades of combined experience in microbial safety testing. Supported by a state-of-the-art laboratory, we utilize certified culture media, phase-contrast microscopy, validated S9-free workflows, and real-time PCR instrumentation to ensure both sensitivity and specificity in detection—meeting or exceeding regulatory expectations.
Fast Turnaround Time with Rigorously Validated Protocols
Time-to-market is essential in biologics and cell-based therapies. Our streamlined protocols, rapid PCR workflows, and 28-day culture monitoring procedures are optimized for speed without sacrificing accuracy. All methods are fully validated to deliver dependable and reproducible results, supporting your compliance and product release timelines.
Strict Data Confidentiality and Intellectual Property Protection
We adhere to strict data protection policies, enforce comprehensive non-disclosure agreements (NDAs), and maintain secure, audit-ready documentation systems. Your proprietary formulations and testing outcomes are safeguarded at every stage of the testing process.
Global Regulatory Compliance and Market Readiness
Our mycoplasma test reports are designed for immediate inclusion in regulatory dossiers under USP <63>, EP 2.6.7, JP, and ICH Q5A guidelines. Whether you are targeting approvals from FDA, EMA, NMPA, or other global health agencies, our testing services meet the highest international standards for biologics and advanced therapy products.
To request testing or a complimentary consultation contact Nikopharmad
Partner with Nikopharmad for Trusted Mycoplasma Testing
By choosing Nikopharmad for your mycoplasma testing requirements, you gain a reliable, globally accredited partner with a proven track record in microbiological safety. Our scientific excellence, regulatory alignment, and commitment to data integrity ensure your biologics reach patients safely, efficiently, and in full compliance with global expectations.
Conclusion
Together, the cultivation and PCR methods provide a comprehensive framework for detecting mycoplasma contamination in biopharmaceutical production and research settings. The cultivation method offers confirmation of viability and biological relevance, while PCR ensures rapid and highly sensitive screening. When performed in accordance with pharmacopeial guidelines, including validated sensitivity, specificity, and rigorous use of positive and negative controls, these methods serve as essential safeguards in the assurance of microbiological quality and patient safety in biologics manufacturing.